How Should Physicians and Pharmacists Collaborate to Motivate Health Equity in Under-served Communities?
AMA J Ethics. 2021;23(2):E117-126. doi: 10.1001/amajethics.2021.117.
Hope French, PharmD Candidate 2023
Shenandoah University School of Pharmacy
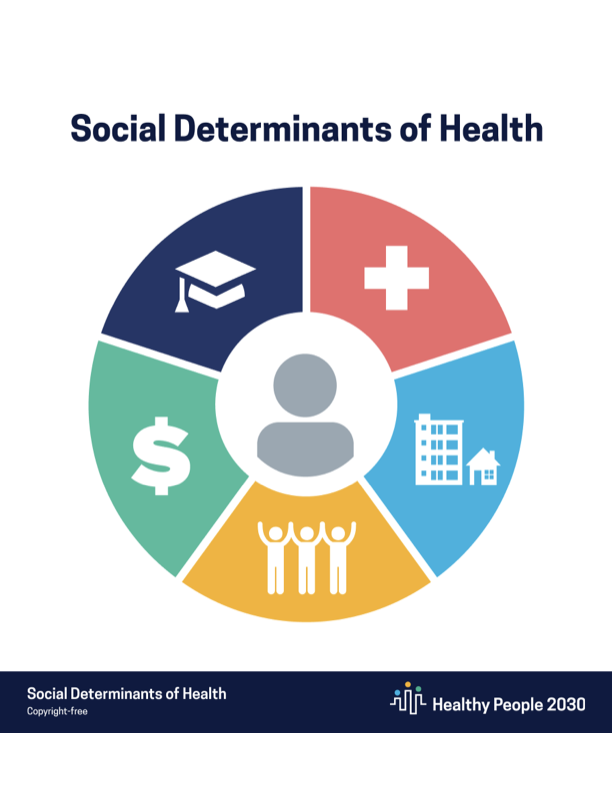
Charitable pharmacists are able to have a large impact on patients in under-served populations or with barriers to accessing healthcare1. They, and those who work with them, are in a position to identify potential social determinants of health: economics, education, environment, access to healthcare, and social and community context.2 By providing medications at reduced or no copay as well as pharmacy services, these pharmacists are able to remove some of these barriers and improve patient outcomes. Another way that charitable pharmacies can impact patient care is by offering therapeutic interchange. When a patient’s medication has a high cost, the pharmacist can change the prescription to a lower cost, therapeutically similar med, immediately if a collaborative practice agreement (CPA) is in place. CPAs are utilized to benefit the patient and reduce barriers associated with cost, adherence issues, disease management, and more.
The AMA Journal of Ethics published a case commentary recently, discussing social determinants of AJ, an 85-year-old man.3 AJ has multiple chronic diseases, does not have insurance, and knows limited English. Because of his health and personal history, AJ already faces several barriers to effective healthcare. When a pharmacist working under a CPA began reviewing AJ’s records, they discovered duplicate ACE inhibitor therapy and that his A1C was 11%. When discussing these findings with AJ, the pharmacist realized that AJ was concerned about the cost of his medications and therefore was not taking the full doses of his insulin.
This is an opportunity for charitable pharmacies to collaborate with other healthcare professionals to improve care in patients with chronic disease states.3 In the United States, approximately 60% of the population has a chronic disease.3 These diseases can include hypertension, diabetes, obesity, and others. Due to disparities of healthcare and other social determinants of health, many under-served communities are disproportionately affected by these chronic disease states.4 Pharmacists are able to have a significant impact on these populations as one of the most accessible healthcare providers in these communities. One study examined the impact of intervention by a pharmacist compared to regular intervention on patients with uncontrolled diabetes.4 In the group with pharmacist intervention, the median decrease in A1C was 1.6%, compared to 0.4% in the standard intervention group. It is also worth noting that the patients who received the majority of the benefit were of nonwhite race/ethnicity. Examples like this demonstrate that pharmacists are essential in working with other clinical providers, especially in under-served populations.
References:
- Access to Care: Development of a Medication Access Framework for Quality Measurement
- https://health.gov/healthypeople/priority-areas/social-determinants-health
- How Should Physicians and Pharmacists Collaborate to Motivate Health Equity in Underserved Communities?
- Jameson JP, Baty PJ. Pharmacist collaborative management of poorly controlled diabetes mellitus: a randomized controlled trial. Am J Manag Care. 2010;16(4):250-255.