Together, we’re making a difference in both Public Health and Population Health
Kay Olapo, PharmD Candidate, 2022, Belmont University College of Pharmacy
A well known phrase in healthcare is population health, but it is important to clarify the impact of medication access for both population health and public health. Public health is the science and art of preventing disease, prolonging life, and promoting health through the organized efforts and informed choices of society, organizations, public and private communities, and individuals.² For example, authorization of COVID-19 vaccines by the FDA through assessing phase 2 and phase 3 trials are ways the government enforces their authority and implements public health.
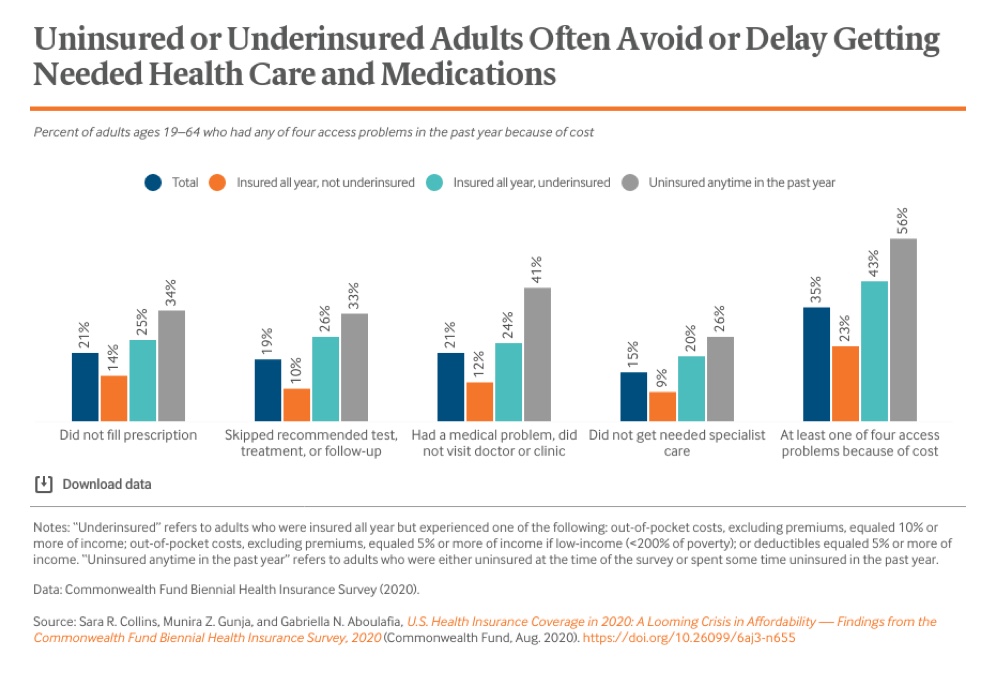
The above example illustrates a public health issue: the comparison of insured, underinsured and uninsured who avoid or delay care. As previously stated, being underinsured and uninsured costs the healthcare system upwards of $3.5 billion to $10.3 billion annually.³ This is one area that we strive to mitigate. When nonprofit health systems, charitable pharmacies and clinics can order and maintain their own inventory of over 400 of the most needed chronic illness medications, then patients have more direct access to medication. The drugs are dispensed at no cost to eligible patients who can then more adequately manage their disease states to improve health outcomes and reduce the overall cost of healthcare.
Population health focuses on the health outcomes of patient groups, whether geographic or any defined group. These groups are commonly associated with geographic populations such nations or communities, but can also be other groups such as ethnic groups, disabled persons and prisoners.
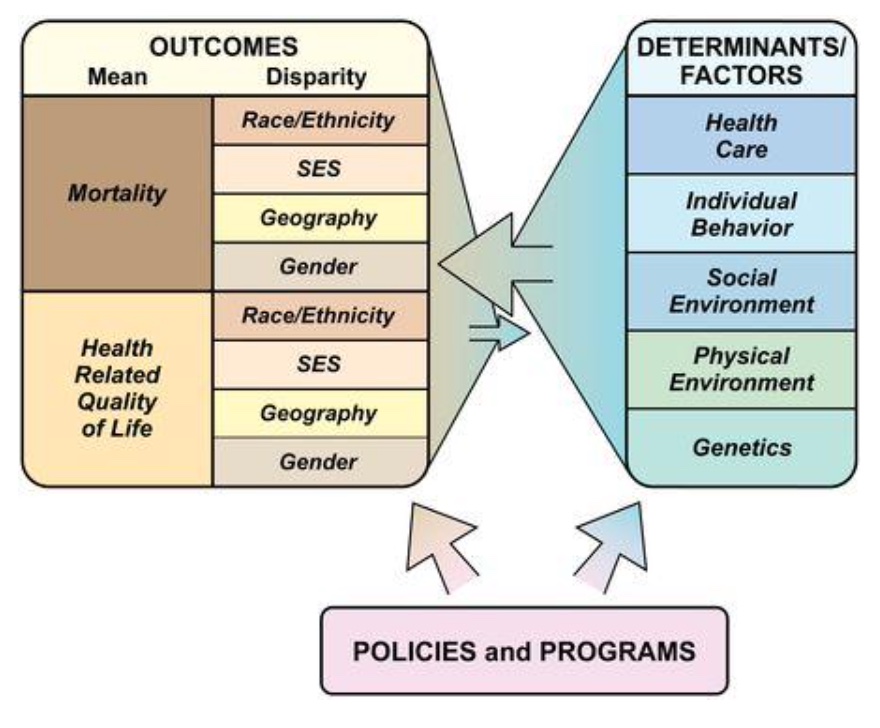
Population health concerns, such as pharmacy deserts, often lead to public health concerns such as poor health outcomes. Pharmacy deserts exemplify a population health concern that sometimes goes unaddressed. For example, patients that are required to travel further to obtain a prescription, due to being located in a pharmacy desert, experience a hardship in obtaining their medication. As a result, those with a low socioeconomic class have less access to prescription medications. This was shown in an article titled ‘Pharmacy Deserts’ Are Prevalent In Chicago’s Predominantly Minority Communities, Raising Medication Access Concerns.¹ It was found in the same study that ranged from 2000 to 2012, that the amount of pharmacies in segregated minority communities were lower compared to segregated white and integrated communities.¹ Due to this, people in underserved populations have higher rates of dyslipidemia, hypertension, diabetes, etc. The lack of pharmacies leads to higher chronic conditions resulting from lack of resources, access, and other health care disparities. The research suggests that addressing healthcare disparities, like pharmacy deserts, through location, allocation, and education will have a positive impact on accessibility and equity.
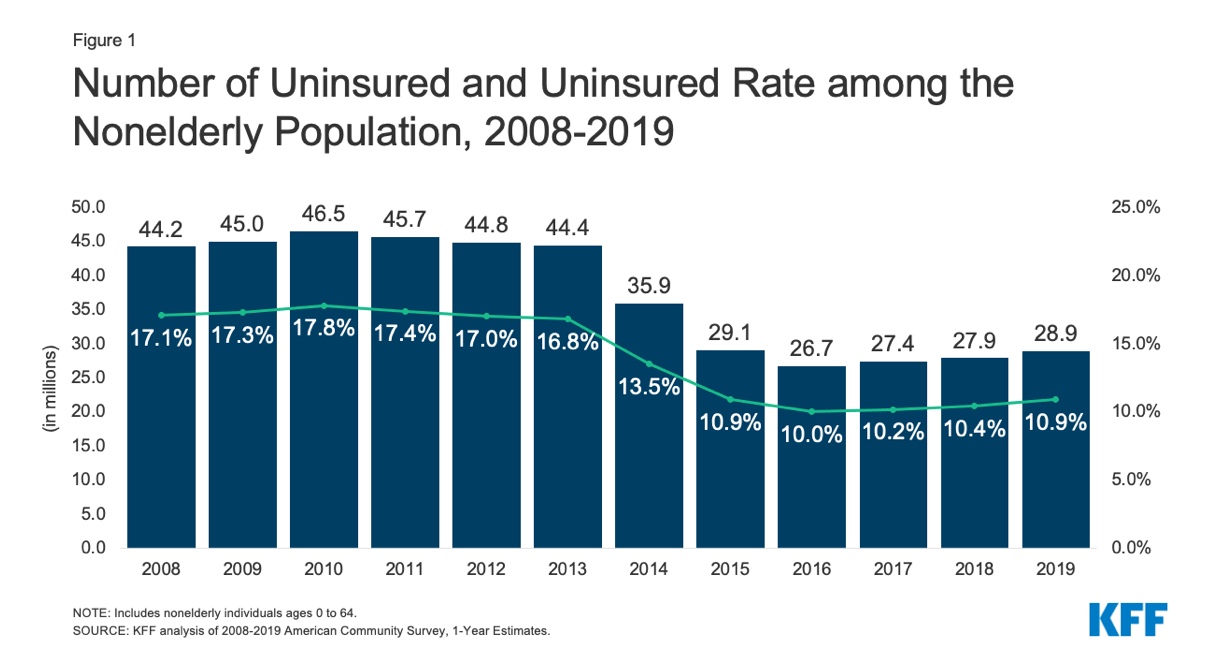
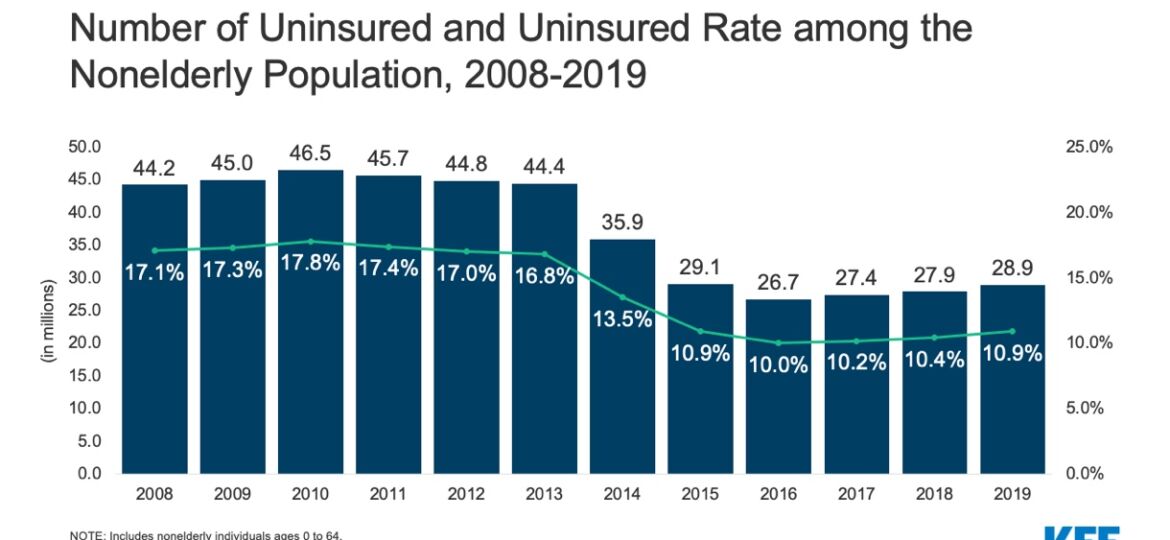
The chart above depicts uninsured rates of the non-elderly population from 2008-2019. While the rate was low in 2016, the data trend shows a slight increase. In addition, 5.4million Americans became uninsured in 2020, likely due to Covid-19. America’s poor population are often found grouped in geographic areas. About three in ten within rural counties (31%) and about one in five within cities reside in concentrated impoverished areas.⁵ We serve this population and assist in the treatment of many uninsured patients.
A goal of population health is to treat patients that have healthcare disparities due to, but not limited to, their geographic area. Charitable pharmacies and clinics provide an efficient way of attaining crucial prescriptions for patients that reside in pharmacy deserts and concentrated impoverished areas across the US.. Prescriptions that in turn allow charitable care to go further and help more people in need by lowering readmission rates. Together, we reach uninsured patients who may not have the ability to afford medication or insurance due to lack of income or eligibility. Charitable pharmacies, clinics and sitributors represent an opportunity to interrupt the cycle and reverse the trends of poor medication adherence, poor health outcomes, increased service utilization and increased health care cost across the nation.
References:
Diana M. Qato, Martha L. Daviglus, Jocelyn Wilder, et al. ‘Pharmacy Deserts’ Are Prevalent In Chicago’s Predominantly Minority Communities, Raising Medication Access Concerns. Measuring Community Health. 2014; 6/04/2021
Public Health 101 Series. Centers for Disease Control and Prevention. Updated September 22, 2020. Accessed June 4th 2021. https://www.cdc.gov/training/publichealth101/public-health.html
Estimated Cost of Treating the Uninsured Hospitalized with Covid 19. Kaiser Family Foundation. Published April 07,2020. Accessed June 4th 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/estimated-cost-of-treating-the-uninsured-hospitalized-with-covid-19/
Austin W, Jordan H, Hillary B, et al. Consulting. Dispensary of Hope-Advisory Board White Paper. 2016; 6/10/2021
Kim P, Juliana Menasce H, Anna B, et al. Demographic and Economic trends in urban, suburban, and rural communities. Pew Research Center. May 2018. Accessed June 15th 2021. https://www.pewresearch.org/social-trends/2018/05/22/demographic-and-economic-trends-in-urban-suburban-and-rural-communities/